Article No. 6
Evaluation of Stress Urinary Incontinence
Author
 Dr. Nishita Shah
Dr. Nishita Shah
MBBS, DNB
Reviewed by
 Dr. Priti Vyas
Dr. Priti Vyas
INTRODUCTION
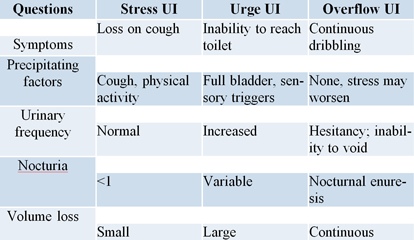
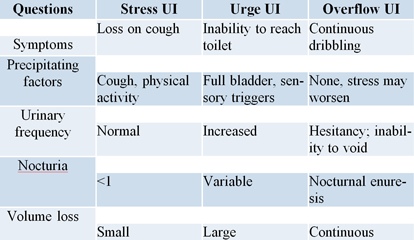
Urinary incontinence (UI), according to the International
Continence Society, is defined as the involuntary loss of
urine. The most commonly recognized subtypes of UI are
stress urinary incontinence (SUI), urge urinary incontinence
(UUI), and mixed urinary incontinence (MUI).
History taking & Examination: To
categorize as SUI, UUI /overactive bladder syndrome (OAB),
MUI or overflow UI and to help understand the underlying
cause and identify factors that may impact treatment
decisions:
- Duration
-
Most bothersome one
- Frequency
- Precipitants
-
Other factors: previous pelvic surgeries, comorbid
conditions, current medications, for her urinary problems
or some other indications, symptoms of pelvic organ
prolapse, defecatory dysfunction, pelvic pain and sexual
dysfunction
-
Medical, neurological, obstetric and gynaecological
history
Examination:
-
General and abdominal examination to rule out enlarged
bladder or other abdominal mass. Careful assessment of
oestrogen status and any associated genitourinary
prolapse; and Pelvic floor assessment with digital
examination of the rectum and vagina.
-
A cough stress test: Any leakage of urine
with coughing vigorously; with bladder empty or filled,
with patient supine or standing; is considered positive
test. Interpretation: A positive empty supine stress test
indicative of intrinsic sphincter deficiency.
-
Hypermobility: Quantify the degree of
hypermobility by measuring the angle of deflection from
horizontal of the swab inserted into the urethra during
cough or Valsalva maneuver. Interpretation: When urine
leakage occurs without urethral hypermobility intrinsic
sphincter deficiency is suspected.
Other Modalities for Diagnosis:
-
Patient questionnaires
- Voiding diaries
- The pad test
-
Urinalysis with urine culture sensitivity
-
Post-voiding residual volume: Amount of urine that remains
in the bladder after voiding. Both bladder outlet
obstruction and detrusor underactivity contribute to the
development of PVR.
-
Imaging: To understand the anatomical and functional
abnormalities
-
Urodynamics: Determines the functional
status of the bladder and urethra
-
Uroflowmetry : A free-flow void into a
recording device, quantifying the volume of urine
passed, the maximum (Qmax) and average rate of
urine flow (Qave), voiding time,
flow time and time to maximum flow .Qave
in women usually ranges from 17 to 24 ml/s.
-
Pressure flow studies (PFS) –Voiding
Cystometry
: Detrusor pressure is measured during controlled bladder
filling and subsequent voiding with measurement of flow
rate.
-
Videourodynamics: Involves use of
contrast medium instead of saline, to assess position and
mobility of bladder neck in addition.
-
Ambulatory Urodynamics:Functional test of the lower urinary tract, using
natural filling and reproducing the patient’s
everyday activities; Indication: as in neurogenic lower
urinary tract dysfunction
Normal urodynamic parameters in women

Urethral Pressure Studies
-
Leak point pressures : Detrusor leak point pressure
(DLPP)- lowest detrusor pressure at which urine leakage
occurs in absence of either detrusor contraction or
increased abdominal pressure
Abdominal leak point pressure (ALPP) or Valsalva leak
point pressure (VLPP)- intravesical pressure at which
urine leakage occurs due to increased abdominal pressure
in the absence of a detrusor contraction -measurement of
urethral function or outlet competence.
-
Urethral Pressure Profilometry (UPP)- continuous fluid
pressure needed to just open a closed urethra. Maximum
urethral pressure (MUP)- maximum pressure of the measured
profile
Maximum urethral closure pressure (MUCP)- maximum
difference between urethral pressure and intravesical
pressure

-
Urodynamics should not be routinely carried out when
offering conservative treatment for UI and with defined
clinical diagnosis of pure stress UI.
Indications: when findings may change the choice of surgical
treatment
prior to surgery for UI
symptoms of OAB
history of previous surgery
suspicion of voiding difficulty
Guidelines on indications for urodynamics are not widely
implemented, resulting in practice variation in workup of
women with UI.
At present, the urodynamic outcomes hardly influence the
choice of treatment.
Stress testing with reduction of the prolapse should be done
in women with high grade pelvic organ prolapse but without
the symptom of SUI.
Conclusion
UI is a common symptom that can affect women of all ages,
with a wide range of severity and nature. Hence extent and
interpretation of its evaluation must be with a defined
protocol- identify the type of incontinence, understand its
effect on the quality of life and expectations from the
treatment, associated problems, and thorough and effective
counseling so that a consensus is met as regards the
treatment to be planned.
Today’s necessity is to perform more studies on
current diagnostic modalities like urodynamic investigation
and how to combine different diagnostic modalities in a way
to to create a more uniform algorithm for UI and make
evaluation less cumbersome and easy to access.