
- CALL US TODAY!
- 022-35114384 / 022-35114385 / 9022361841

- EMAIL US
- [email protected]
Article No. 5


INTRODUCTION
Preeclampsia is seen in 5% of pregnancies & 20-25% in cases of chronic hypertension. PIH was a term popularized by Dr. Jack Pritchard. Now preferably the term gestational hypertension is used.
The ACOG Task force on Hypertension (HT) in pregnancy chose to continue using the classification scheme first introduced in 1972 by the college & modified in 2000 report of National High Blood Pressure Education Programme Working Group. There are 4 categories of Hypertension in pregnancy:
Postpartum Hypertension: It is important to remember that preeclampsia can first develop in the postpartum period. Women need to be instructed at discharge to report to the health care provider if there is any headache, visual disturbance or epigastric pain.
There is also a phenomenon called ‘Late postpartum hypertension’ – women who are normotensive in pregnancy and develop mild HT – 2 weeks to 6 months postpartum. Little is known about this entity.
After diagnosis the next step is evaluation of the mother & fetus.
For maternal evaluation the tests recommended by ACOG are; CBC, Platelet count, Serum Creatinine, Liver function test & Urine Protein.
For fetal evaluation the tests recommended are; USG for fetal weight, AFI, NST & Biophysical profile.
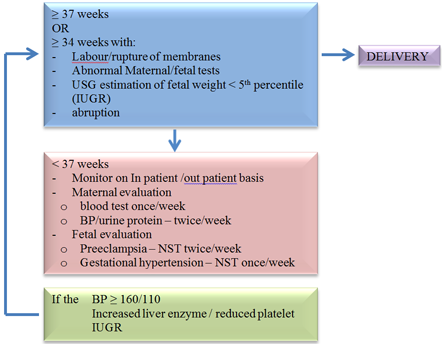
Gestational age & maternal & fetal findings are the criteria for taking decisions in management of preeclampsia.
For mild HT / preeclampsia with BP less than 160 / 110, antihypertensive drugs are not recommended. They reduce the BP but also reduce fetal growth. Bed rest & salt restriction are also not currently recommended. Also, for ‘mild preeclampsia’ Magnesium Sulphate has no role.
On the other hand severe hypertension ≥ 160/110 in pregnancy has to be treated to prevent potential cardiovascular complication (CHF, MI) renal failure & cerebrovascular accidents. Hydralazine, Labetalol & Nifedipine are equally effective & safe. Any of these can be used.
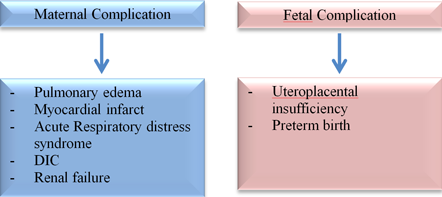
Severe hypertension can cause serious complications to the mother & fetus.
For women with severe preeclampsia at or beyond 34 weeks of gestation delivery soon after maternal stabilization is recommended.
For women with chronic hypertension who are at increased risk of adverse pregnancy outcomes (eg. History of early preeclampsia), initiating administration of daily low dose aspirin 60 – 80 mg beginning in the late first trimester is suggested.
.png)
Expectant Management allows the baby to be delivered at a more advanced gestational age. It reduces NICU requirement, Respiratory distress syndrome, Necrotising enterocolitis, intraventricular haemorrhage. However, it increases the chances of IUGR or SGA babies.
If severe preeclampsia occurs before 24 weeks, then the patient should be delivered after stabilising the maternal condition. Neonatal outcome of expectant management is poor.
Patients with preeclampsia can be delivered by LSCS/vaginally depending on the obstetric situation.
The most important consideration in management of women with hypertension in pregnancy is the safety of the woman & her fetus. The second is delivery of a mature newborn that will not require NICU.