Article No. 9
Medical Management of Male Infertility
Author
 Dr Rana Choudhary,
Dr Rana Choudhary,
MOGS Youth Council Member
DNB, FCPS, DGO, DFP, MNAMS Associate Consultant, Ankoor
Fertility Clinic, Mumbai
Reviewed by
 Dr. Kedar Ganla,
Dr. Kedar Ganla,
MOGS Youth Council Mentor
MD, DNB, FCPS, DGO, DFP
Director, Ankoor Fertility Clinic, Mumbai
INTRODUCTION
Infertility is regarded as ‘Male Factor’ when an
alteration in sperm concentration and/or motility and/or
morphology is present in at least one sample of two sperm
analyses, which comply with the World Health Organization
(WHO) 2011 guidelines. It is partly responsible for
infertility in 50% of these couples.Therefore identifying
the pathology and treating it may allow couple to improve
their fertility potential and conceive naturally.
Factors affecting choice of therapy
-
Age of couple & duration of infertility
- Severity of OATS
-
Past illness(mumps-related orchitis)
-
Reversible, correctable gonadotoxic factors like exposure
to hot environmental conditions (furnacesetc)
-
Antioxidants trial already given
-
Socioeconomic status
-
Psychosocial pressure
Aims of medical therapy
-
To improve count, motility and morphology of sperms.
-
Increase rates of spontaneous conception.
-
Lower rates of miscarriages due to DNA abnormalities in
sperm.
Specific Medical therapy
Non specific or Emperical therapy
1.Hormonal agents
2.Antioxidants
Inspite of doing IVF/ ICSI, there is high incidence of
implantation failure and early pregnancy loss. If the DNA of
sperm is damaged, it will result in a poor pregnancy
outcome. Between 30% to 80% of idiopathic male subfertility
cases are considered to be due to effects of oxidative
stress on sperm.
Spermatozoa are vulnerable to ROS because their plasma
membrane and cytoplasm contain large amounts of
polyunsaturated fatty acids.
Eg. Glutathione 250mg/day, Lycopene 4-8g/d, Vit E
400-800mg/d, Vit C.
3.Spermvitalisers
Energises the sperms (improves motility) and increases
fertilization. May assist in sperm maturation and some have
antioxidant properties.
Eg . L & Acetyl carnitine 1g thrice a day
Coenzyme Q10 100-300mg/d
Carnitines are used by spermatozoa for mitochondrial
membrane stabilisation and energise the sperm.
4. Nutritional supplements
May be of some benefit in nutritionally depletedpatients.
Eg. Multivitamins with zinc,selenium, folic acid and B12.
Conclusion
Further reading:
-
-
Chronic scrotal fungal dermatitis –
-
Can cause thickening of scrotal skin &
local temperature.
-
Treatment – Topical antifungal and steroids.
-
Genital tract infections – Leucocytospermia (WBC
count in semen > 1 x 106 / ml). Prevalence 10-20%.
-
Semen culture
-
Common organisms – Streptococcus fecalis, E
coli, Chlamydia trachomatis,
Ureaplasmaurealyticum.
-
Because of the difficulty of culturing,
Doxycycline 200mg/day is given for 15days on
empirical basis
-
Antibiotics maybe added later as per culture
reports,eg. – Fluoroquinolones 0.5 –
1g / day, Cotrimoxazole or Erythromycin 1.5-2
g/day for 2-3 weeks.
-
Culture negative patients – Anti
inflammatory therapy and frequent ejaculations
-
Refractory leucocytospermia – Sperm washing
and IUI.
-
Immunological infertility –
-
Oral steroids - To suppress antibody production,
but efficacy not confirmed by double blind
randomised trial.
-
Pregnancy rates are 0 to 44%, with maximum
pregnancy seen after treatment for more than 3
months.
-
Treatment - Tab predinisolone 5mg, thrice a day
for 10days with tapering of dose.
-
Chronic epididymo-orchitis
-
Clinical evidence of chronic filarial
epididymo-orchitis like enlarged adherent
epididymis, thickened cord etc.
-
Treatment – Diethylcarbamazine (DEC) 100mg
thrice a day for 20 days + Doxycycline 100mg twice
a day for 10 days, followed by low dose steroids.
-
Androgens - Administered at a dose that will not
influence the pituitary gonadal axis, may have direct
stimulatory effect (in low doses) on spermatogenesis
or influence sperm transport and maturation, with no
effect on sperm motility. Helpful in hypogonadotropic
hypogonadism.
-
Eg. Mesterolone 25 thrice a day.
-
Testosterone undecanoate80 – 160mg / day
-
Antiestrogen - Inhibit the negative feedback effect of
estrogen by blocking estrogen receptors in
hypothalamus and thus gonadotrophins.
FSH & LH stimulate sertolileydig cells and
improve spermatogenesis.
-
Aromatase inhibitors increase FSH. In older men
with so-called late-onset hypogonadism, aromatase
inhibitors may emerge as an attractive alternative
for traditional testosterone supplementation to
improve testosterone levels.
-
Who will benefit? -Idiopathic male infertility
-
Who will not be benefited? -High Baseline FISH,
Severe OATS,Azoospermia
-
Eg. Clomiphene citrate 25 mg / day
-
Tamoxifen citrate 10-20mg/ day
-
Aromatase inhibitors – Inhibit peripheral
conversion of testosterone to estrogen and enhance
spermatogenesis.
-
Normal testosterone (T)/ Esterogen (E2) is 1: 16
-
Low T/E ratio indicates high Aromatase
activity
-
Useful in a subpopulation of patients with low
T/E2 ratio(eg. obese men)
-
EgLetrozole 2.5mg daily orally
-
Gonadotrophins – Helpful in men with idiopathic
infertility (subclinical endocrinopathy) with normal
hormonal levels.
-
Eg HCG 1500 IU or HMG 37.5 – 75 IU thrice a
week
-
InjrFSH 300 IU daily followed by 3-6 cycles of IUI
followed by ICSI.
-
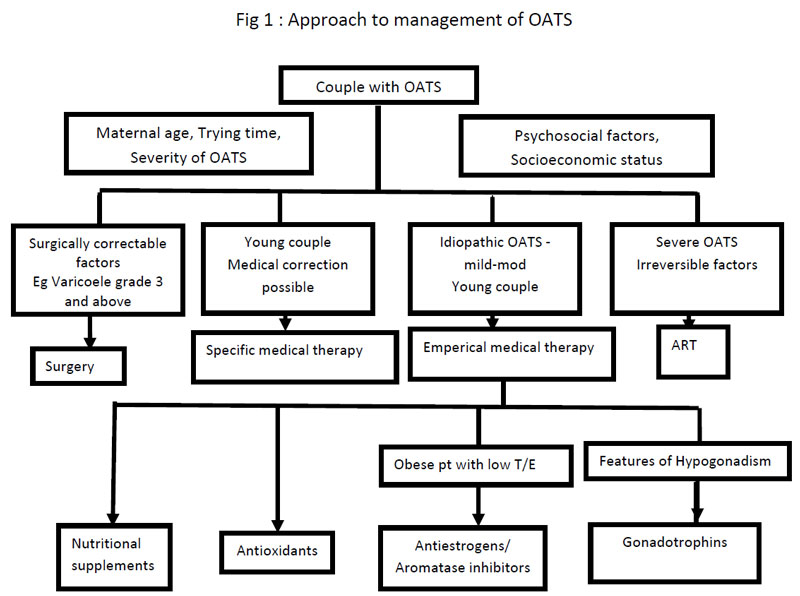
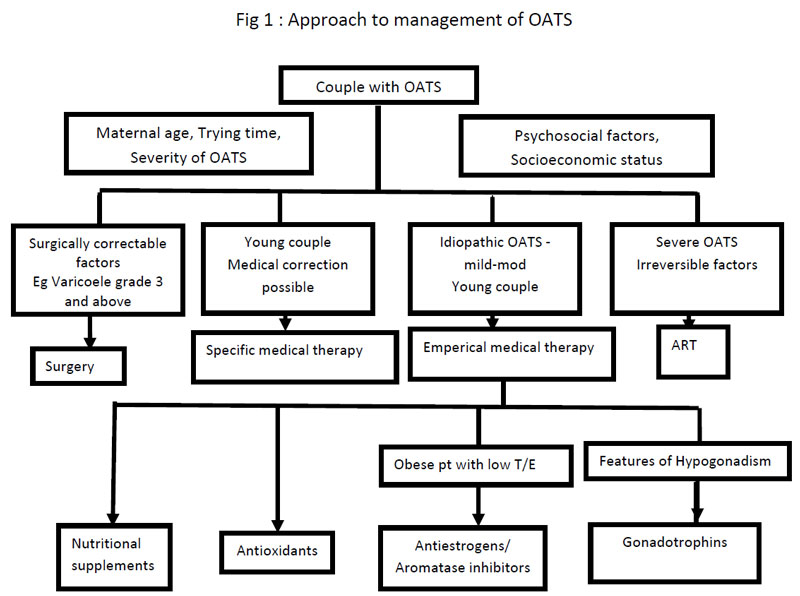
Give a very clear road map of therapy
-
Individualised treatment, with timeline and endpoints
established beforehand
-
Treatment should be of atleast 3 months, followed by
repeat semen analysis.
-
Give realistic expectations.
-
Do not waste time and money over medical therapy if
circumstances call for assisted reproductive therapy.
-
Willem de Ronde et al. Aromatase inhibitors in men:
effects and therapeutic optionsReprodBiolEndocrinol.
2011; 9: 93. doi: 10.1186/1477-7827-9-93 .
-
Patel DP et al . Hormone-Based Treatments in
Subfertile Males. CurrUrol Rep. 2016 Aug;17(8):56.
doi: 10.1007/s11934-016-0612-4.
-
Owen RC et al .Testosterone supplementation in men: a
practical guide for the gynecologist and
obstetrician.CurrOpinObstet Gynecol. 2015
Aug;27(4):258-64. doi: 10.1097/GCO.0000000000000192.
-
Ho CC Treatment of the Hypogonadal Infertile Male-A
Review. Sex Med Rev.2013 May;1(1):42-49. doi:
10.1002/smrj.4.