
- CALL US TODAY!
- 022-35114384 / 022-35114385 / 9022361841

- EMAIL US
- [email protected]
Article No. 1


Female pelvic organs have two portals of entry: one natural and the other surgically created. T he vaginal approach has always been the hallmark of the gynaecologic surgeon. Dr Harry Reich who pioneered the first laparoscopic hysterectomy in 1989 recommended Vaginal hysterectomy when it can be safely carried out in preference to Laparoscopic Hysterectomy. Laparoscopic Hysterectomy should be considered as an alternative to Abdominal hysterectomy1. In 2009 the American College of Obstetricians and Gynaecology Committee2 concluded that the vaginal route is associated with better outcomes and fewer complications than the laparoscopic or abdominal hysterectomy. A Cochrane Review3 of 34 randomized controlled trials of abdominal, laparoscopic and vaginal hysterectomies concluded that vaginal hysterectomy has the best outcomes and when its not possible, laparoscopic hysterectomy should be considered. Laparoscopic route although minimally invasive (numbers or size of abdominal cuts) is still more invasive then the vaginal route. When science indicates/recommends/directs task becomes easy to discuss the choice of Hysterectomy route.
Common indications for NDVH include:
Uncommon indications include:
Contraindications-
Common-
Uncommon-
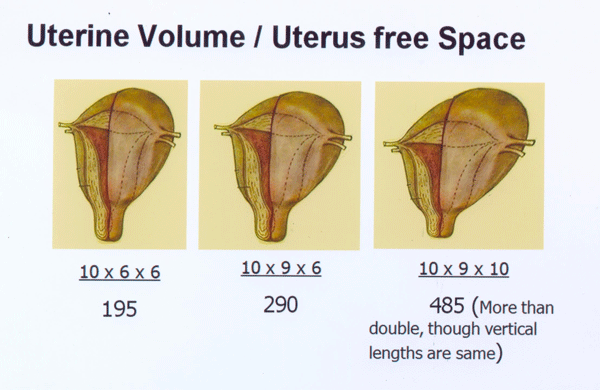
When the uterine volume is less than 300cc the operator should consider vaginal hysterectomy. ACOG recommends VH if the uterine size is 12 weeks or less or the uterine volume is 285cc or less. Pre operative USG is imperative as it excludes adnexal masses, confirms uterine size, estimated clinically gives the details on fibroids, thus reassuring the surgeon.
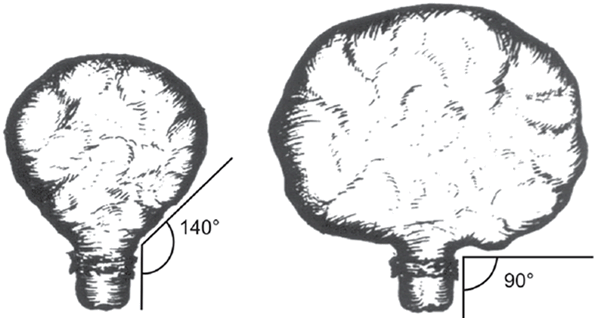
Volume includes all 3 uterine dimensions whereas size in weeks is based on Fundal height only. For example, two uteri may have the same fundal height, however they may have different breadths and/or antero posterior diameter and hence grossly different volumes. Formula for calculation of uterine volume is length x breadth x AP dimension x 0.5426.
Lets discuss difficulties in performing Non Descent Vaginal Hysterectomies and how they can be over come-
Nulliparity/No prolapse or descent - Every freely mobile uterus without pelvic pathology has some physiological descent which permits start of vaginal hysterectomy .In order to arrive at a decision, one must seize the opportunity to examine under anesthesia any woman undergoing a conservative surgery ,like laparoscopy or hysteroscopy in a nulliparous lady to look for vaginal descent and keep a note of it. As long as the uterus is less then 12 weeks size or 250-300cc volume, nulliparity per say should never contraindicate vaginal hysterectomy.
Enlarged Uterus or Uterine Fibroid - Uterine enlargement could occur due to adenomyosis, uterine fibroids, or myometrial hyperplasia due to dysfunctional uterine bleeding. On examining the patient under anaesthesia, traction is applied on the cervix, if the fundus descends and disappears in the pelvis, and is not palpable per abdomen then the vaginal route should not pose a problem. In addition, after securing the uterine arteries, debulking methods such as bisection, vaginal myomectomy, coring reduce the uterine volume and makes hysterectomy easy.
History of previous abdominal or pelvic surgery - Previous Caesarean Sections or myomectomy in no way contraindicates vaginal hysterectomy. Sheths uterocervical broad ligament space7 or the lateral window should be utilized as the adhesions in this area are less dense and firm and the bladder is not in direct contact with the cervix. This anatomical space is as follows- anterior wall consists medially of the under surface of bladder and laterally the anterior leaf of broad ligament. The posterior wall consists of the uterocervical surface. Laterally, the space is bounded by a tangential line joining the maximal bulging point on the uterine body and cervix. Medially the space ends when the bladder comes in close contact with the uterocervical surface thickening at the level of bladder pillars. Almost all adhesions are present in the central 3/5th and not usually the lateral 1/5th.
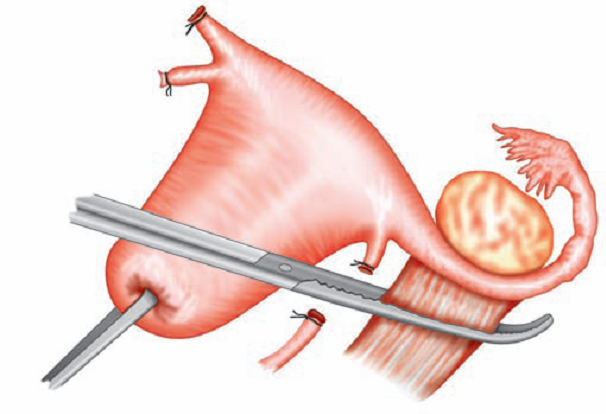
Need for oophorectomy - The principal in such cases is to cut the round ligaments as laterally from the uterus and clamp the infundibulopelvic ligament to perform salpingo oophorectomy . Sheth reported 97% success while performing prophylactic oophorectomy in more then 1500 cases.
Conclusion
Thus the vaginal route can be used for a wide variety of indications for hysterectomy. Based on the available evidence, in the best interest of the patients only a genuine contraindication via the vaginal route should indicate LAVH or abdominal hysterectomy. The gold standard for decision making in the absence of contraindications is examination under anaesthesia. In todays consumer-driven society if vaginal surgery was marketed to patients as “scarless surgery”, perhaps it would become more popular.
References