
- CALL US TODAY!
- 022-35114384 / 022-35114385 / 9022361841

- EMAIL US
- [email protected]
Article No. 8


The management of preterm labour involves identification of high‐risk women, prevention and treatment. The aim is to prevent preterm labour in women at high risk or to delay delivery in a woman who has already presented with preterm labour, allowing the clinicians time to administer corticosteroids for lung maturity and antibiotics if preterm labour is associated with rupture of membranes, thereby improving the neonatal outcome.
IDENTIFICATION OF WOMEN AT RISK
Identification of women at high risk of preterm labour poses a major challenge. However the ability to identify women at risk for preterm birth has improved significantly over the past few years. This is due to the introduction of a number of predictive tests as follows.
Risk Factor Scoring. A number of risk factors for preterm birth have been identified which can be divided as modifiable and non-modifiable. Several scoring systems have been developed based on these historic/epidemiologic risk factors and daily habits in an attempt to predict women at risk for preterm birth. The single greatest risk factor for preterm birth is a history of a prior unexplained spontaneous preterm delivery.1
Sonographic Cervical Length Measurement
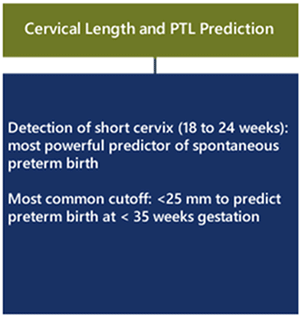
A strong inverse correlation exists between residual cervical length as measured by transvaginal ultrasound and preterm birth. The detection of a short cervix by transvaginal ultrasound at 18 to 24 weeks gestation is the most powerful predictor of spontaneous preterm birth.2 (Figure 1)
Other specific tests and monitoring modalities
Salivary Estriol, bacterial vaginosis testing, home uterine activity monitoring (HUAM) and Fetal fibronectin measurement have been proposed to assess a woman’s risk of preterm delivery. Salivary Estriol, bacterial vaginosis testing and HUAM in recent studies have shown to have no benefit in predicting PTL The only test that is currently FDA approved and recommended by The American College of Obstetricians and Gynecologists (ACOG) for this indication is the measurement of fetal fibronectin (fFN) in cervicovaginal secretions. Elevated levels of cervicovaginal fFN (defined as > 50 ng/mL) at 22-0/7 through 34-6/7 weeks of gestation are associated with an increased risk of preterm birth. The primary value of this test lies in its negative predictive value (99% of patients with a negative fFN test will not deliver within 7 days), which may prevent unnecessary hospitalization and medical intervention.
Ultrasonographic cervical length assessment and fetal fibronectin appear to be similar in predictive ability, and the combination of both in a high-risk population maybe of value. However, further research is needed in this area. 3
PREVENTION OF PRETERM LABOUR
1.Progesterone supplement
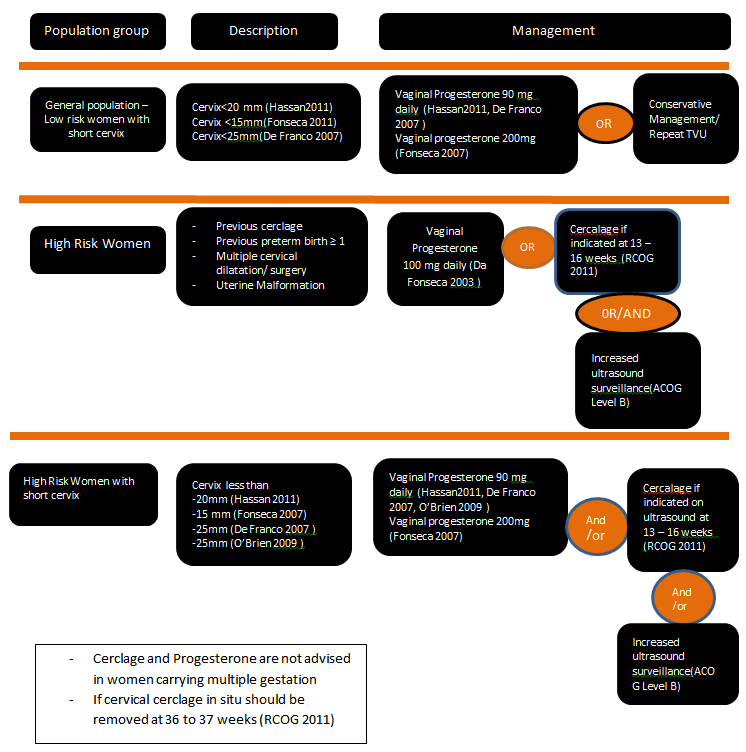
The most important single advance of the past decade has been the introduction of progesterone supplementation for the prevention of premature labor. In 2011, the US Food and Drug Administration (FDA) for the first time has approved the use of progesterone supplementation (hydroxyprogesterone caproate) during pregnancy to reduce the risk of recurrent preterm birth in women with a history of at least one prior spontaneous preterm delivery1. Preventive treatment with progesterone can lower the rate of preterm birth in high-risk groups by more than 30% . The optimal progesterone formulation, route of delivery, and dose for the prevention of preterm birth has not yet been determined1.It is now recommended that all pregnant women who have either a prior history indicating increased risk or current, asymptomatic cervical insufficiency should receive progesterone supplementation until 34 completed weeks of gestation.
Recommendations for progesterone supplement

2. Role of cervical encerclage
It has been suggested that cerclage may be helpful if the cervix is short in women with history suggesting cervical incompetence. Cerclage may not be helpful in those women who have a short cervix without a history of incompetence.
The ACOG Practice Bulletin on Cerclage for the Management of Cervical Insufficiency in 2014 suggests cerclage placement may be indicated in women with a singleton pregnancy who have a history of one or more second trimester pregnancy losses with painless dilation and without labor or abruption placenta, history of prior cerclage for painless dilatation, and physical examination of cervical dilatation in the second trimester.5 (FIGURE 3)
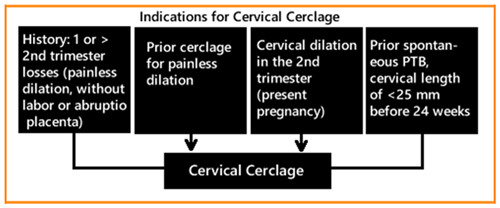
ACOG level B recommendation mentions that cerclage may increase the risk of preterm birth in women with a twin pregnancy and an ultrasonographically detected cervical length less than 25mm and is not recommended.2
In all asymptomatic women, who present with membranes at or protruding past the external cervical os, an emergency cerclage should be considered to reduce the risk of preterm delivery. Insufficient evidence exists to assess whether progesterone and cerclage together have an additive effect in reducing the risk of preterm birth in women at high-risk for preterm birth.4 (FIGURE 4)
3. Other interventions
Other interventions, such as pharmacotherapy with indomethacin or antibiotics, activity restriction, or supplementation with omega-3 fatty acids are not recommended as clinical interventions for women with an incidentally diagnosed short cervical length4Management of these women includes reduction of activity level, work, or travel, relocation, increased surveillance, and administration of corticosteroids.3
CONCLUSION
Preterm labour is a multifactorial condition associated with a high risk of morbidity and mortality, particularly at early gestational ages. Prevention is directed towards identification of women at risk and comprises screening and treatment for bacterial.
REFERENCES