Page 26 - Demo
P. 26
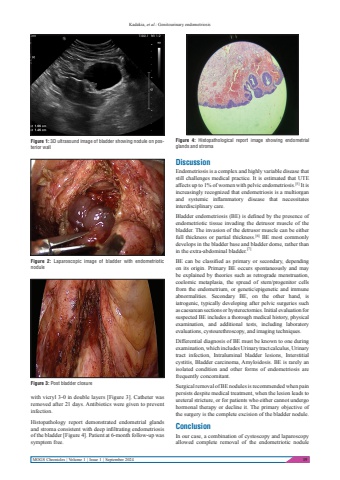
Kadakia, et al.: Genitourinary endometriosisMOGS Chronicles | Volume 1 | Issue 1 | September 2024 19with vicryl 3-0 in double layers [Figure 3]. Catheter was removed after 21 days. Antibiotics were given to prevent infection.Histopathology report demonstrated endometrial glands and stroma consistent with deep infiltrating endometriosis of the bladder [Figure 4]. Patient at 6-month follow-up was symptom free.DiscussionEndometriosis is a complex and highly variable disease that still challenges medical practice. It is estimated that UTE affects up to 1% of women with pelvic endometriosis.[5] It is increasingly recognized that endometriosis is a multiorgan and systemic inflammatory disease that necessitates interdisciplinary care.Bladder endometriosis (BE) is defined by the presence of endometriotic tissue invading the detrusor muscle of the bladder. The invasion of the detrusor muscle can be either full thickness or partial thickness.[6] BE most commonly develops in the bladder base and bladder dome, rather than in the extra-abdominal bladder.[7]BE can be classified as primary or secondary, depending on its origin. Primary BE occurs spontaneously and may be explained by theories such as retrograde menstruation, coelomic metaplasia, the spread of stem/progenitor cells from the endometrium, or genetic/epigenetic and immune abnormalities. Secondary BE, on the other hand, is iatrogenic, typically developing after pelvic surgeries such as caesarean sections or hysterectomies. Initial evaluation for suspected BE includes a thorough medical history, physical examination, and additional tests, including laboratory evaluations, cystourethroscopy, and imaging techniques.Differential diagnosis of BE must be known to one during examination, which includes Urinary tract calculus, Urinary tract infection, Intraluminal bladder lesions, Interstitial cystitis, Bladder carcinoma, Amyloidosis. BE is rarely an isolated condition and other forms of endometriosis are frequently concomitant.Surgical removal of BE nodules is recommended when pain persists despite medical treatment, when the lesion leads to ureteral stricture, or for patients who either cannot undergo hormonal therapy or decline it. The primary objective of the surgery is the complete excision of the bladder nodule.ConclusionIn our case, a combination of cystoscopy and laparoscopy allowed complete removal of the endometriotic nodule Figure 2: Laparoscopic image of bladder with endometriotic noduleFigure 1: 3D ultrasound image of bladder showing nodule on posterior wallFigure 3: Post bladder closureFigure 4: Histopathological report image showing endometrial glands and stroma